INTRODUCTION
Cerebrospinal fluid (CSF) rhinorrhea is characterized by the leakage of CSF through the nose. This condition can arise from both traumatic and non-traumatic causes, with head trauma being responsible for approximately 80% of cases [
1]. Common symptoms of CSF rhinorrhea include watery rhinorrhea, a metallic taste, and increased leakage when lowering the head. The diagnosis involves high-resolution computed tomography (CT) and magnetic resonance imaging, along with nasal endoscopy [
1].
Conservative management is the initial approach, with most cases resolving within 7 to 10 days [
2,
3]. If rhinorrhea persists or worsens after 7 to 14 days of conservative treatment, surgical treatment must be considered. In recent years, endoscopic intranasal management has become the preferred surgical treatment for CSF rhinorrhea. This approach is preferred over intracranial surgical repair due to its lower morbidity and higher success rates, particularly for uncomplicated CSF leaks located at the anterior or posterior ethmoid roof and within the sphenoid sinus [
2,
3].
When repairing a leakage site endoscopically, materials such as autologous fat tissue, muscle fascia, and bone fragments, including the ethmoid plate, can be used to repair the defect site [
4,
5]. However, the use of fat tissue or muscle flaps may lead to complications, including infection at the donor site, hematoma, or wound dehiscence [
5-
7].
Therefore, in this paper, we would like to present two cases of CSF leakage repair surgery performed simply using TachoComb.
CASE REPORTS
Case 1
A 58-year-old woman presented at our hospital with a complaint of clear, runny nasal discharge that had begun 3 days prior. Her medical history included hypertension, and she had undergone a Simpson Grade I cranial tumor removal via right supraorbital craniotomy 7 years earlier. Additionally, she had sustained an injury to the left temporal area by bumping it against the corner of a cupboard 3 months before her visit. The rhinorrhea was characterized by a clear, watery discharge from the left nasal cavity, which increased when she lowered her head and decreased when she raised it. The patient also noted that the discharge had a salty taste when swallowed. At the time of her visit, the nasal discharge was showing signs of improvement. However, she reported a headache that affected her entire head and a fever of 37.9°C.
There were no findings suggestive of CSF leakage. However, brain CT revealed a newly developed, large pneumocephalus measuring approximately 2.1×7.0 cm on the axial view. Additionally, there was a suspicious bone defect at the posterior wall of the central Onodi air cell, which appeared to communicate with the suprasellar area (
Fig. 1). Following the diagnosis of pneumocephalus, the patient was prescribed absolute bed rest and underwent lumbar drainage. Nevertheless, on the 9th day of hospitalization, the patient’s level of consciousness declined from alert to confused, coinciding with a recurrence of left-sided watery rhinorrhea. A follow-up paranasal CT scan showed an increase in the volume of pneumocephalus. Consequently, surgical intervention was planned to repair the defect at the posterior sphenoid sinus using nasal endoscopy and navigation.
Through the transseptal approach, the periosteal and perichondrial flaps were elevated. A portion of the posterior septal bone was then excised and preserved. To improve visibility, the opening of the sphenoidal anterior wall was enlarged. Utilizing a navigation device to verify the location, the Onodi air cell was accessed from above the sphenoid sinus, and a pinpoint-sized CSF leak was identified on the posterior wall of the Onodi cell. The previously harvested posterior septal bone was used to cover the defect, but it was smaller than the defect itself. Consequently, further reconstruction was performed, which involved reinforcing and packing the area with TachoComb (
Fig. 2). After ensuring there was no additional CSF leakage, both nasal cavities were packed with Nasopore, and the operation was concluded.
To prevent postoperative CSF leakage, lumbar drainage was maintained, and the patient was kept on bed rest for 7 days. There were no specific symptoms such as rhinorrhea or postnasal drip following the operation. On the 9th day after surgery, the Nasopore was removed, and it was confirmed that the reconstruction site and flap were intact (
Fig. 3). The patient was monitored on an outpatient basis for any signs of CSF leakage until the 16th postoperative day and continues to be followed up in the outpatient clinic.
Case 2
A 60-year-old man presented to our hospital complaining of a headache that had started 1 day ago. The patient had a history of hypertension and had undergone endoscopic sinus surgery 1 month before admission. He described the headache as a throbbing sensation affecting his entire head, accompanied by a fever of 38.2°C and bilateral clear rhinorrhea.
Pneumocephalus measuring approximately 4.8×1.0 cm on the axial view was detected in both frontal areas on brain CT (
Fig. 4). Nasal endoscopy, however, revealed no specific findings beyond old blood clots. Given that the headache persisted on the 13th day of admission, surgical exploration via nasal endoscopy was planned.
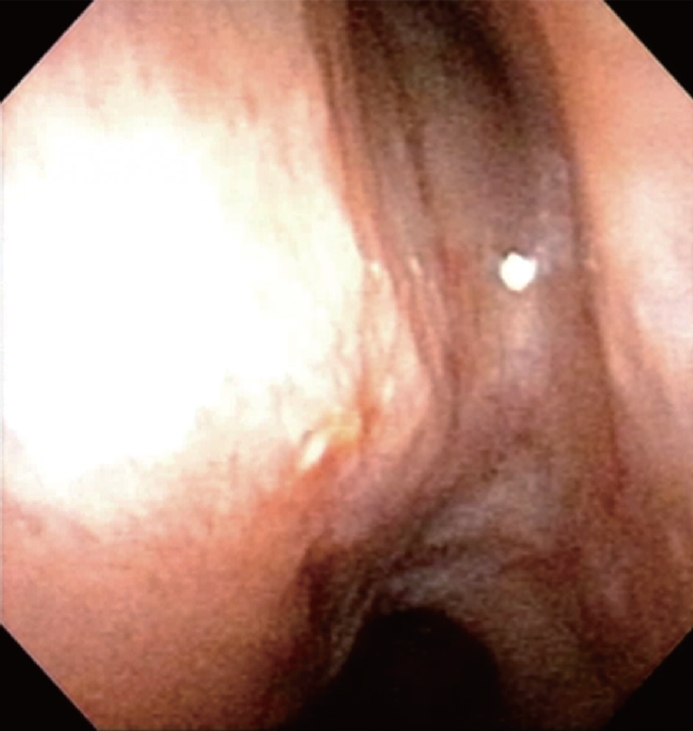
Using a nasal endoscope, dural damage and CSF leakage were confirmed at the base of the right frontal lobe (
Fig. 5). Mucosa was harvested from the middle turbinate to create a free mucosal graft. This graft was then placed over the CSF leakage site, and the area surrounding the defect was extensively covered and compressed with TachoComb.
The patient was required to undergo absolute bed rest for 5 days to prevent the recurrence of CSF leakage following surgery. Since there were no further incidents of postnasal drip or rhinorrhea, the patient was deemed fit for discharge on the 17th postoperative day.
The patient attended follow-up appointments at the outpatient clinic for 2 years postoperatively, during which no symptoms, including CSF leakage, were observed. Thereafter, he was lost to follow-up.
DISCUSSION
The initial treatment for CSF leakage is conservative care, but surgical management should be considered if there is no response to conservative treatment for more than a week or if there is a defect in the skull base [
1].
Since the introduction of functional endoscopic sinus surgery, intranasal endoscopic repair has become the preferred method over intracranial surgical repair due to its higher success rates and reduced morbidity in selected cases [
8]. An intranasal endoscopic approach is often favored for closing simple CSF fistulas located in the anterior or posterior ethmoidal cells and sphenoid sinuses, while an intracranial approach may be more suitable for addressing complex CSF leaks, such as those associated with extensive comminuted fractures of the anterior cranial base [
4].
A variety of graft materials are available for the repair of endoscopic CSF leaks; these include autografts (such as fat and bone), allografts (such as acellular human dermis), free mucosal grafts, vascularized grafts, and various glues or sealants (including dural sealants and fibrin glues like TachoComb). Recent studies have demonstrated that the use of a vascularized pedicled nasoseptal flap can reduce the incidence of postoperative CSF leaks [
6,
7,
9]. Therefore, nasoseptal flaps have become the preferred option for repairing large skull base defects or managing high-flow leaks [
10].
Recent studies have reported the success rate of nasoseptal flaps to be between 89% and 95% [
6,
7,
9]. The causes of postoperative CSF leaks after nasoseptal flap repair include inadequate coverage due to the flap size being smaller than the defect size, flap dehiscence resulting from excessive debridement, and flap death caused by preoperative radiation therapy [
6,
11].
TachoComb, the material we utilized in these cases, is a collagen matrix coated with activated thrombin and fibrinogen. It has been employed in various medical fields, including otolaryngology, endoscopic surgery, and operations involving the thyroid, liver, lungs, blood vessels, and nervous system. Specifically, TachoComb is applied to prevent pleural defects or pneumothorax during lung surgery, to minimize postoperative bleeding in abdominal procedures, and to serve as a dural substitute in neurosurgery.
In this study, we used TachoComb in conjunction with free grafts such as nasoseptal bone and turbinate mucosal flap in the cases described. Unlike other studies that have employed underlying grafts or vascular flaps [
6,
7,
9], our approach involved placing free grafts, like septal bone or turbinate mucosal flap, over a portion of the CSF leakage defect. We then extensively covered the defect and its surrounding area with TachoComb to ensure thorough coverage and prevent flap dehiscence. Additionally, this technique mitigates the risk of flap necrosis by utilizing free grafts rather than relying exclusively on underlying grafts or vascular flaps. We suggest that this method offers otolaryngologists a straightforward and effective solution for sealing CSF leaks while minimizing donor site morbidity.
As demonstrated in the two cases presented herein, no postoperative CSF leakage was observed in this study. It is believed that TachoComb aids in the adherence of the nasoseptal flap to the defect, thereby preventing flap dehiscence. Additionally, it provides extra coverage to areas that may not be sufficiently covered by the flap alone.
However, regarding the specific surgical method and approach, various factors such as the location and size of the defect, the surgeon’s preference, and the patient’s individual characteristics should be taken into account. Additionally, it is believed that further studies are required to reach a consensus on the optimal surgical method.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



